Safely Detox from Suboxone at Ingrained Recovery
Suboxone is a drug that’s commonly prescribed by doctors to treat opioid addiction. While it’s very effective, it requires comprehensive treatment, including close supervision, counseling, and behavioral therapy. But those things sometimes don’t happen in tandem, especially in some community-based outpatient settings. So while it’s helpful in managing opioid withdrawal symptoms, improper use can leave you asking yourself: How can I detox from suboxone?
Ingrained Recovery applies scientific research in our efforts to help clients overcome opioid addiction, including medication-assisted treatment and other evidence-based therapies. Under our close medical supervision, you can end your suboxone addiction safely and with minimal incidence of physical discomfort, aches, and pains of the typical opioid withdrawal process.
This page will explain how people become addicted to suboxone and what you can expect during the recovery process.
Suboxone Treatment and How it Breaks Physical Dependence on Opioids
Suboxone is a prescription medication that contains two active ingredients:
- Buprenorphine: A partial opioid agonist that helps with reducing drug cravings and lessening withdrawal symptoms without the same effect as other opioids.
- Naloxone: An opioid antagonist that deters people from misusing their suboxone dose. If suboxone is injected instead of taken as prescribed, the naloxone blocks the opioid effects.
Suboxone is effective in Medication-Assisted Treatment (MAT) plans. At Ingrained, it’s combined with counseling, behavioral therapy, and holistic therapies that support recovery. It’s also a safe medication for most people, with few adverse or allergic reactions.
While it’s very effective, suboxone itself can lead to physical dependence if used in ways other than prescribed by a medical professional. As the body adjusts to the less harmful replacement opioid, buprenorphine, the doctor will develop a tapering schedule and gradually reduce the suboxone dosage until the client can discontinue the medication.
Get Effective Treatment Programs at Ingrained Recovery

Choosing Suboxone Detox Treatment with Medical Supervision
Suboxone detox might be the most challenging phase for those struggling with opioid dependence. But a medical detox is both safe and effective, setting the tone for a successful recovery.
Whether you became addicted to prescription painkillers after a surgery or accident or self-medicated a mental health condition to relieve your pain, you should not attempt to quit suboxone without the help of a medical detox facility.
You receive continuous monitoring and care throughout your treatment with a medically supervised detox. Our team of addiction medicine specialists will keep watch over your emotional and physical well-being through the entire detox process.
Going Cold Turkey Is a Bad Way to Start Addiction Treatment
Abruptly stopping suboxone is risky. Many who try to quit opioids without the assistance of a medical detox center relapse shortly after they experience withdrawal symptoms, putting them in harm’s way. Taking suboxone leads to a host of withdrawal symptoms when you stop using it, even if you started taking it to stop taking other opioids.
In a treatment facility, medical staff will prevent withdrawal symptoms from worsening by providing prescriptions once time triggers withdrawal symptoms.
Suboxone Withdrawal Symptoms
Many start to feel the emotional and physical symptoms within a few hours of the last dose of suboxone. Not all people will have severe symptoms, but the severity is almost impossible to predict. Without receiving detox in a supervised setting, the symptoms can become overwhelming. That increases the likelihood of a relapse.
Get Proven Detox and Rehab Options at Ingrained

Physical Symptoms of Suboxone Withdrawal
Here are some of the most prominent physical suboxone withdrawal symptoms:
- Muscle aches and pains
- Abdominal cramps
- Nausea and vomiting
- Diarrhea
- Sweating
- Chills or goosebumps (similar to the flu)
- Fatigue
- Low energy
- Insomnia
- Sleep difficulties
- Runny nose
- Watering eyes
- Tremors or shakes
- Rapid heart rate
- Headaches
The severity depends largely on the dosage, duration of the suboxone addiction, and individual metabolism.
Psychological Symptoms of Suboxone Withdrawal
Next, let’s look at the emotional and psychological symptoms one might experience:
- Opioid drug cravings
- Anxiety
- Nervousness
- Depression or low mood
- Irritability
- Anger
- Agitation or restlessness
- Lack of focus/concentration
- Mood swings
- Feeling hopeless or overwhelmed
- Nightmares
- Vivid dreams
Medical supervision gives you access to around-the-clock medical care to help alleviate these symptoms.
Suboxone Addiction: Expected Detox Timeline
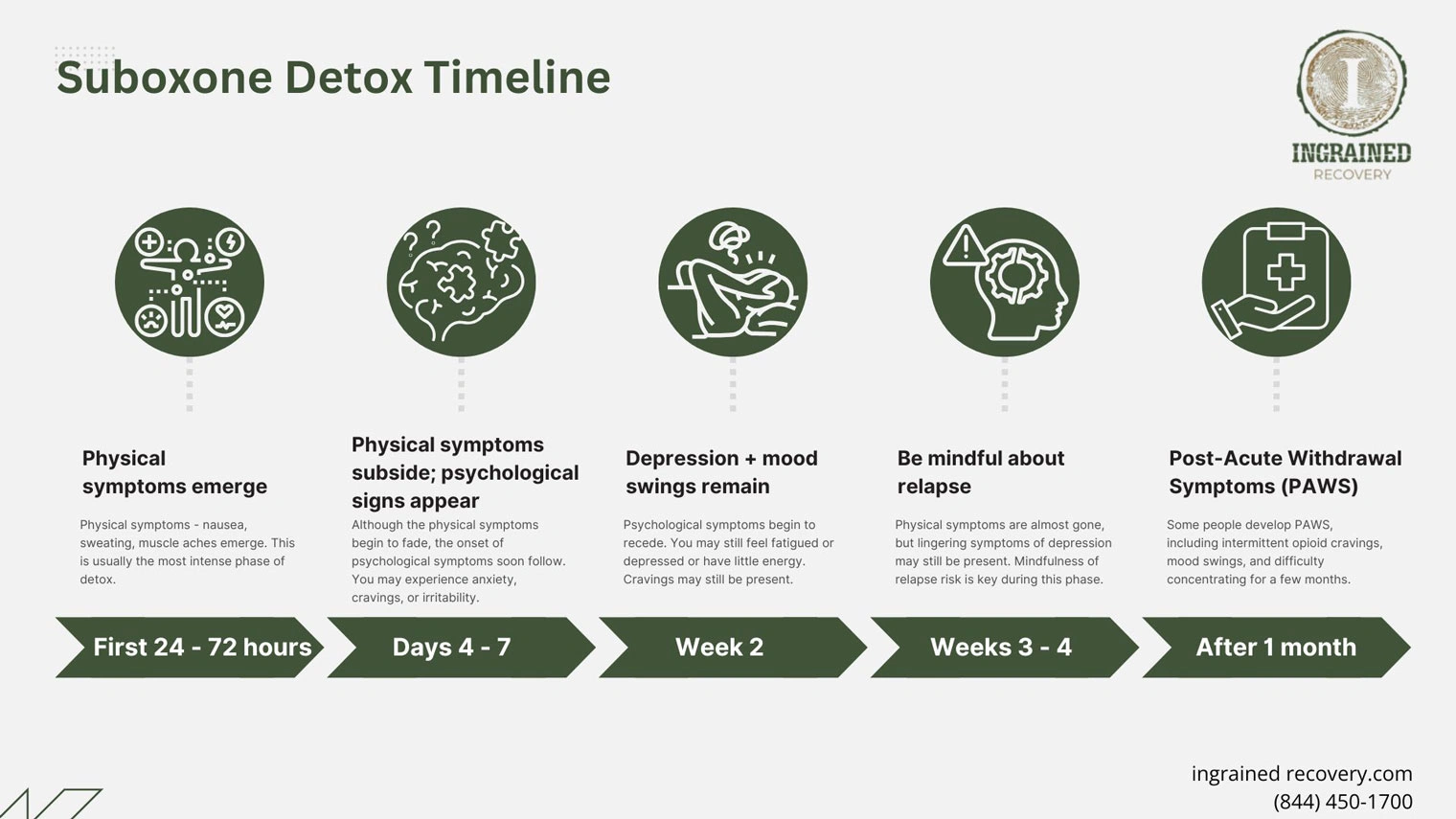
How long it takes to start to feel better after the drug addiction withdrawal symptoms subside can vary from one person to the next. Our suboxone withdrawal timeline gives you a general idea of what to expect as you discontinue suboxone.
As you read through a description of each point on the timeline, you’ll read about Brea, a fictional young woman (representative of anyone struggling with opioids) going through suboxone detox. She started taking the partial opioid agonist to recover from an opioid addiction to prescription painkillers after an injury. Now, Brea’s current suboxone dose will be her last. She’s on the way to addiction treatment and suboxone detox.
Phase 1: Physical Symptoms the First 24 - 72 Hours After Last Substance Use
Most physical symptoms appear within the first few hours after the last opioid use. The initial phase of recovery, undergoing detox, means the first of the symptoms we described earlier, pains, nausea, sweating, and muscle aches, emerge. This is usually the most intense phase of detox. Remember that a professional detox and treatment program will provide medication to reduce withdrawal symptoms.
Brea’s Journey: Brea stopped taking suboxone. Understanding the withdrawal timeline, she was sure she’d have no problems. But several hours after last taking suboxone, her opioid receptors were unoccupied for the first time in a few years. The last dose wore off, triggering nausea and vomiting. The addiction specialist gave her medication to calm her stomach and fluids to prevent dehydration. She was safe, relatively comfortable again, and able to continue her opioid addiction journey.
Phase 2: Days 4 - 7 Mental Health Symptoms Appear
Although the physical pains begin to fade a little after a few days, you may still have a few lingering symptoms. During this time, the onset of psychological symptoms will soon follow. You (or your loved one) may experience anxiety, cravings, or irritability.
Brea’s Journey: After a few days, Brea became physically stable, but she became agitated and cried out of frustration and anger. She grew frustrated with the nurses. She met a kind counselor who taught her some deep breathing exercises. Although she wasn’t ready for any real conversation with the counselor, she appreciated learning the calming techniques.
Phase 3: Depression and Mood Swings Remain for 2 Weeks
Psychological symptoms begin to recede in about a week. You may still feel fatigued or depressed or have very little energy. Cravings may still be present. You may feel like you’ve hit a brick wall, but long-term recovery takes time and persistence. Keep your support system on speed dial and talk to them when you feel like you need help. If you are in treatment at Ingrained, we will be there for you during this critical time.
Brea’s Journey: Brea made it through the highs and lows of her moodiness, but she soon felt a fog of unrelenting despair. She felt like she’d lost her best friend when she gave up her medication. Now she felt alone and unable to cope with her feelings.
A therapist started working with Brea, helping her learn about the true cause of her addiction. It turned out that the accident that had caused her injury remained imprinted on her as unresolved trauma. Together, the therapist and Brea started working on reducing the impact of that traumatic experience on her life.
Phase 4: Cravings Persist in Weeks 3 -4; Attend Support Groups to Avoid Relapse

You’re making great progress by the time you reach weeks 3 and 4, but you’re not out of the woods yet. Physical pangs are almost gone, but lingering symptoms of depression may still be present. Mindfulness of relapse risk is key during this phase. Your counselor will ask you to attend support groups and will have started helping you to develop the coping mechanisms to help prevent relapse during this challenging phase.
Brea’s Journey: Brea continued to flourish in her addiction treatment program at Ingrained. Still, she continued to have pangs, times when she longed for her opioid medication. She knew that if she took it again, it would take the edge off the last shreds of the suboxone withdrawal symptoms that had started shortly after entering detox.
Despite the cravings, Brea held firm and continued working on the coping tools, attending group therapy and 12-step support groups, and individual counseling. She especially loved the equine therapy, even though she’d grown up in Atlanta and had never met a horse before. The ranch setting was quiet, her room was comfortable.
She was safe, even when the cravings still washed over her.
Phase 5: Post-Acute Withdrawal Symptoms Require Good Coping Strategies
The worst suboxone withdrawal symptoms will be behind you in about 5 weeks. Some people develop Post-Acute Withdrawal Symptoms (PAWS), including intermittent opioid cravings, mood swings, and difficulty concentrating for the next few months. You will apply the coping tools you learned in your suboxone addiction treatment program to real life and continue following your recommended program.
Brea’s Journey: Brea left Ingrained with a newfound understanding of the trauma that had led to her injury and addiction. Perhaps more importantly, she left with a new commitment to sobriety. From suboxone detox to the day she left, she wavered but never had a relapse. Her resolve to get clean and sober and stay that way meant more to her than using opioids ever could.
Ingrained Recovery Works With Major Insurers
We accept both self-pay clients and most major insurance plans. Our admissions team understands that suboxone withdrawal is a very difficult time, so we are here to help. Please feel free to call our admissions team. They will take your contact details and insurance plan information, call your insurer on your behalf, and ensure that you receive the most luxurious and effective care for the lowest out-of-pocket costs.
Up To 100% of Rehab Costs Covered By Insurance
Connect With Ingrained for Suboxone Withdrawal and Recovery
Ingrained offers you a luxurious ranch, where you find privacy, peace, and quiet during your recovery. All our indoor spaces provide a calm atmosphere, while our outdoor spaces encourage new friendships and allow our clients to relax after long days of therapy.
Call our team today to learn how you can get our support with suboxone withdrawal and recovery. We are always glad to help.
